What is it?
Patellar instability occurs when the patella moves out of the groove, towards the outside of the knee. There are two types of patellar instability. The first is traumatic patellar dislocation, which typically occurs during a single twisting or pivoting activity. The second is chronic patellar instability, where the patella continues to slide partly out of the groove (subluxation) with activity. In either case, the MPFL is usually injured or deficient.
WHAT ARE SIGNS AND SYMPTOMS OF A PATELLAR INSTABILITY?
Common symptoms of patellar instability include:
• The patella shifting out of place
• Swelling of the knee
• Difficulty walking
• Difficulty straightening the knee
Diagnosis
In the office, a complete history and physical exam is obtained. The knee is assessed for alignment abnormalities and patellar maltracking. A comprehensive test of all the structures, including specific tests for patellar instability, in the knee is performed. Imaging studies, such as an X-Ray and MRI, may be necessary to confirm the diagnosis.
Treatment
Conservative treatment of patellar dislocations is initially recommended. Such treatments include rest, ice, anti-inflammatories, and physical therapy. Crutches and a knee brace may be used initially to support the unstable patella.
Surgical treatment of patellar instability may be indicated if symptoms continue to persist despite conservative treatment, or if there are mechanical symptoms, such as a loose body causing the knee to lock. In most cases, the injured MPFL cannot simply be repaired.
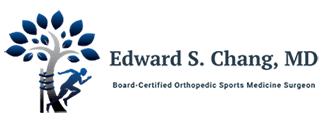
MPFL reconstruction is a surgery aiming to rebuild the medial patellofemoral ligament by using a free tendon graft. Following a diagnostic arthroscopy, a free tendon graft is placed onto the patella and femur by utilizing suture anchors and interference screws. This is typically done in an outpatient setting under regional anesthesia, allowing patients to return home the same day.
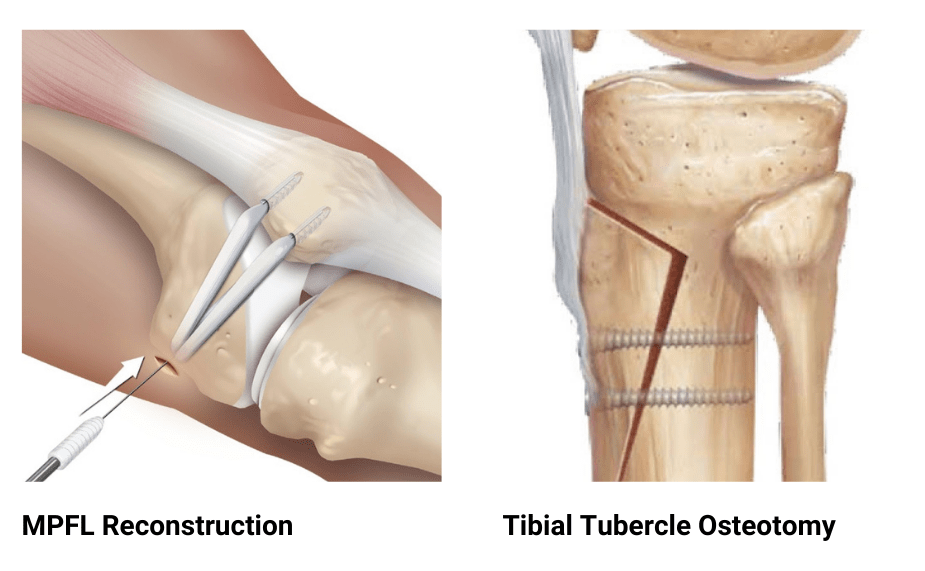
In certain cases, the kneecap is aligned improperly. Soft tissue surgery, such as a MPFL reconstruction, is at risk of failure if the alignment is not addressed. A tibial tubercle osteotomy (TTO) is an open procedure where the tibial tubercle is cut, shifted medially, and held in place by screws. This procedure enhances stability by realigning the patella so that it sits centered into the groove.
RECOVERY
MPFL RECONSTRUCTION
Following surgery, patients are placed on crutches and are allowed to bear weight immediately. Physical therapy begins within the first week of surgery, with emphasis on knee range of motion. At six weeks, the brace is removed and the focus turns to gait training and strengthening. A jogging program is initiated about 3-4 months postoperatively, followed by an agility program at 5-6 months. Patients may generally return to unrestricted activity six months postoperatively.
TIBIAL TUBERCLE OSTEOTOMY
Following surgery, patients are placed in a long hinged knee brace for six weeks and are placed on restricted weight bearing. At four weeks, full weight bearing is permitted. A jogging program is initiated about 3-4 months postoperatively, followed by an agility program at 5-6 months. Patients may generally return to unrestricted activity at six months postoperatively.
MPFL RECONSTRUCTION
The following animation demonstrates a MPFL reconstruction. Following preparation of a free tendon graft, small suture anchors are placed into the patella, and a small socket is drilled into the femur. The graft is then secured to the patella and then placed into the socket. Once the desired tension is obtained, the graft is secured to the femur with an interference screw.
TIBIAL TUBERCLE OSTEOTOMY
The following animation demonstrates a tibial tubercle osteotomy. An incision is made over the patellar tendon and tibial tubercle. Cutting guides are then attached to the tibia, and the optimal cut angle is obtained. An oscillating saw is then used to create the cut. Alternatively, this can be performed free hand. The cut fragment is shifted to obtain the desired correction and then secured back to the tibia with multiple screws.