What is it?
The proximal hamstring complex consists of three muscles: the semimembranosus, the semitendinosus, and the biceps femoris tendon. All three tendons originate from the lower portion of the pelvis, the ischial tuberosity. Proximal hamstring ruptures are rare, comprising five percent of all hamstring injuries. They occur when the hip is suddenly forced into flexion, with the knee in extension. Sports such as water skiing, bull riding, and football are activities that are associated with proximal hamstring ruptures.
WHAT ARE SIGNS AND SYMPTOMS OF A PROXIMAL HAMSTRING RUPTURE?
Common symptoms of proximal hamstring ruptures include:
• Sudden pop in the buttock region
• Bruising and swelling in the back of the thigh
• Difficulty walking
• Numbness and tingling in the lower leg.
Diagnosis
In the office, a complete history and physical exam is obtained. The back of the thigh is examined for any deformity, bruising, or tenderness. The hamstring tendon is evaluated for loss of strength. Imaging studies, such as an X-ray and MRI, are useful in confirming the diagnosis.
Treatment
Conservative management of proximal hamstring ruptures can be performed in partial or incomplete tears. Such treatments include rest, ice, anti-inflammatories, and physical therapy. Crutches are used initially to support the injured extremity.
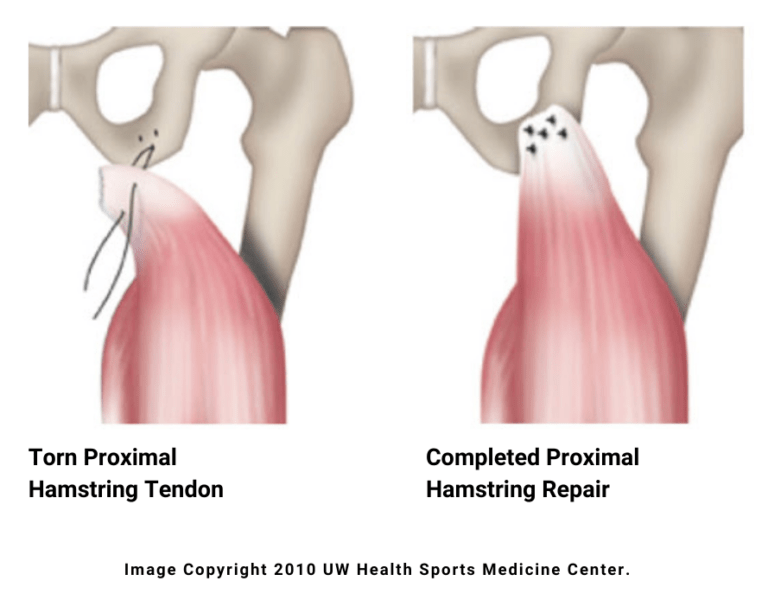
Surgical treatment of proximal hamstring ruptures is recommended when all three tendons are torn, or there is significant retraction with less than three tendons torn. Proximal hamstring repair involves securing the torn tendons to the bone with suture anchors. This is typically done in an outpatient setting under regional anesthesia, allowing patients to return home the same day.
RECOVERY
Following surgery, patients are placed in a hip brace with weight bearing restrictions. At four weeks, the brace is removed, and gait training is initiated. A jogging program begins at 3-4 months postoperatively. Sport specific drills are then initiated at 5-6 months, and patients generally return to sports around 6-7 months postoperatively.