What is it?
The shoulder is a ball and socket joint, consisting of the humeral head (ball) and glenoid (socket). It is the most mobile joint in the body and relies on multiple factors for stability. The labrum is a thick, fibro-cartilaginous tissue that lines the rim of the glenoid. It acts to stabilize the shoulder by deepening the socket and serving as the attachment site for the shoulder ligaments.
Shoulder dislocations occur when the humeral head shifts out of the socket. This generally occurs from a traumatic injury, such as in contact sports like football. 90% of shoulder dislocations occur anteriorly (out the front), and the labrum is almost always torn. Posterior labral tears are rare and often associated with repetitive strain (overuse). This is typically seen in weight lifters or in football offensive linemen. Depending on the patient’s sport or activity and degree of injury, labral tears can put the shoulder at an increased risk of instability or dislocation.
WHAT ARE COMMON SIGNS AND SYMPTOMS OF A LABRAL TEAR?
Common signs of labral tears include:
• Pain deep in the shoulder
• Feeling that the shoulder may slip out
• Repeated dislocations of the shoulder that require it to be put back in
• Difficulty with overhead sports (throwing, spiking, swimming)
Diagnosis
In the office, a complete history and physical exam is obtained. Careful measurements of range of motion, strength, and stability tests of the shoulder are recorded. Oftentimes, diagnostic imaging, such as X-rays and MRI, may be necessary to confirm the diagnosis.
Treatment
Nonoperative management for labral tears is typically recommended as first line treatment. Such treatments include rest, ice, anti-inflammatories, and physical therapy. Physical therapy focuses on strengthening the rotator cuff and scapular muscles to stabilize the shoulder.
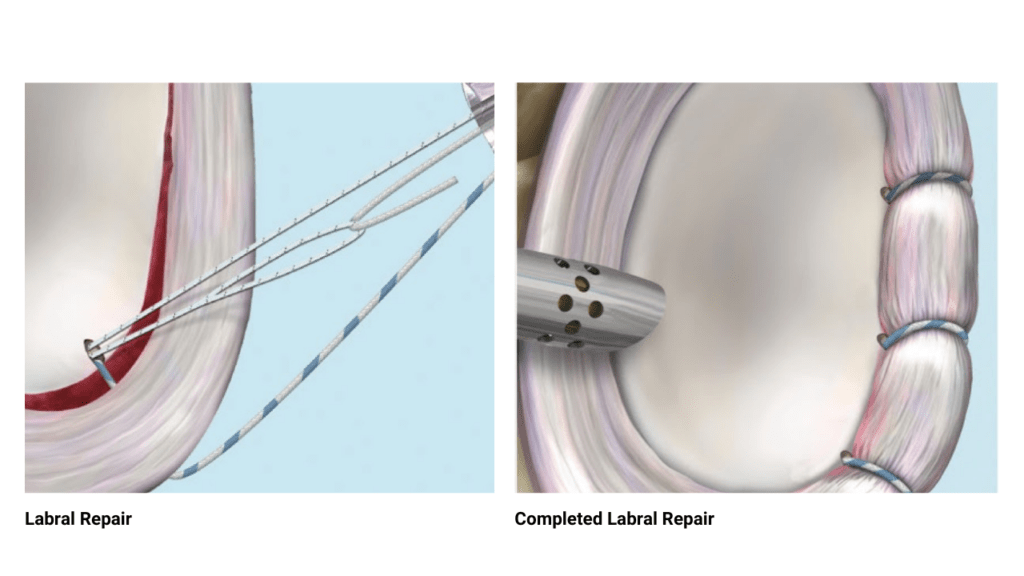
Surgical management generally is recommended in younger patients (< 25 years of age) or in patients with recurrent shoulder dislocations in which physical therapy has failed. Arthroscopic labral repair is a minimally invasive technique that utilizes small incisions to reattach the torn labrum to the bone. This is typically done in an outpatient setting under regional anesthesia, allowing patients to return home the same day. In conjunction with supervised physical therapy, arthroscopic labral repair has been shown to successfully treat shoulder instability and allow athletes to return back to sport.
RECOVERY
Following surgery, patients are immobilized in a sling for six weeks (including sleep for four weeks). Physical therapy begins around three weeks after surgery. Range of motion is then initiated at six weeks, followed by strengthening at 12 weeks. Patients generally return to activities about 5-6 months postoperatively.